Barriers to linkage
Multiple factors may hinder the successful uptake of testing and linkage to care and prevention.
- Quality of post-test counseling including the lack of adequate time for post-test counseling
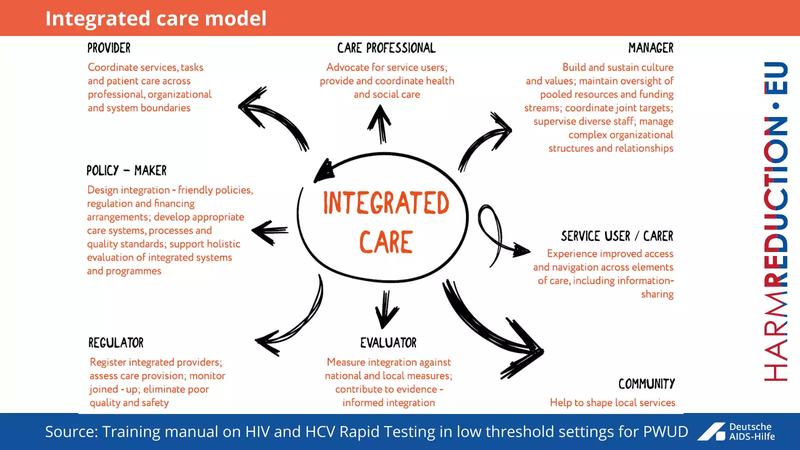
- Lack of coordination between HIV testing and care
- Limited health facility access
- Stigma associated with the health facility
- Inefficient service delivery
- Inadequate patient-provider interaction
- Inadequate program incentives
Multiple factors may hinder the successful uptake of testing and linkage to care and prevention. These include patient-level factors (such as depression, lack of social or family support, and fear of disclosure), as well as structural or economic factors such as stigma and discrimination, distance from care sites, lack of or cost of transportation, and long waiting times at the facility). Hepatitis C and HIV also disproportionally affects individuals with co morbid mental health or substance use issues.
Traditionally, services for hepatitis and HIV, mental health and substance use have been provided by separate clinicians or teams often located in different health facilities, which may contribute to HCV/HIV treatment dropout and/or treatment failure.
KEY MESSAGES
- ENGAGING HIV/HCV PATIENTS IN CARE, IMMEDIATELY AFTER DIAGNOSIS AND CONSISTENTLY THEREAFTER, HAS A PROFOUND IMPACT ON EFFORTS TOWARDS ‘ZERO NEW INFECTIONS’
- MAIN BARRIERS: FINANCIAL (LACK OF INSURANCE OR UNDERINSURANCE, COMPETING SUBSISTENCE NEEDS, FOOD, HOUSING.)
- STRUCTURAL (UNAVAILABLE OR INCONVENIENTLY LOCATED SERVICES, LONG APPOINTMENT WAIT TIMES ETC.)
- ADMINISTRATIVE, PERSONAL (STIGMA OF HIV, SEXUAL IDENTITY, DRUG USE, LACK OF TRUST IN MEDICAL SYSTEM ETC.)


