Integrated care
Integrated Care is a concept bringing together inputs, delivery, management and organization of services related to diagnosis, treatment, care, rehabilitation and health promotion. Integration is a means to improve the services in relation to access, quality, user satisfaction and efficiency.
What is integration
The word “integration” stems from the Latin verb “integer” which means “to complete.” The adjective “integrated” means “organic part of a whole” or “reunited parts of a whole.” It is mostly used to express the bringing together or merging of elements or components that were formerly separate.
“Integration” is used by different people to mean different things. There is no unifying definition or common conceptual understanding of integrated care. The concept of integrated care is strongly shaped by perspectives and expectations of various users in the system, making a unified definition difficult. Interestingly, all definitions converge around highlighting the central role of population and individual needs.
The approaches can be grouped into three broad categories:
individual models of integrated care;
group- and disease-specific models;
population-based models.
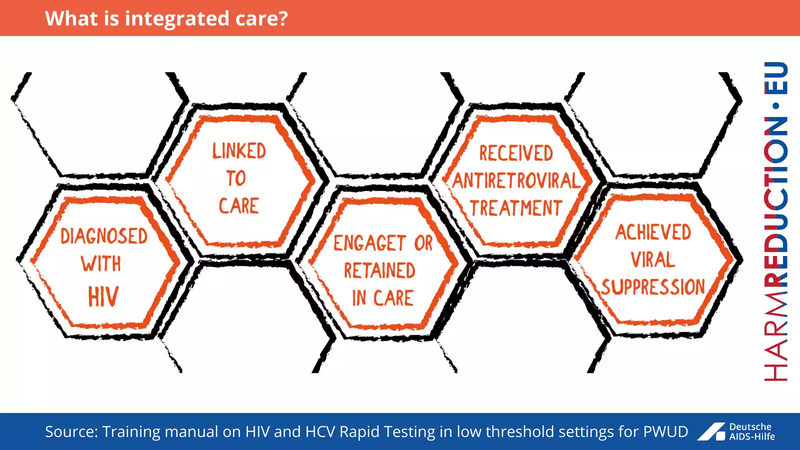
What is integrated care?
Integrated Care is a concept bringing together inputs, delivery, management and organization of services related to diagnosis, treatment, care, rehabilitation and health promotion. Integration is a means to improve the services in relation to access, quality, user satisfaction and efficiency.
Integrated care is care that is person-centred and co-ordinated. For care to be integrated, organisations and care professionals need to bring together the different elements of care that the patient or service user needs. This includes care provided at the same time or at different stages of the care pathway, to address all the patient’s or service user’s needs and to seek to improve their outcomes and experience of care.
Integrated care brings together the different groups involved in patient care so that, from the patient’s perspective, the services delivered are in a consistent and coordinated way. A person’s care may be provided by several different health and social care professionals, across different providers. As a result, people can experience health and social care services that are fragmented, difficult to access and not based around their (or their carers’) needs.
In many cases, the increased efficiency of integrated care also helps control costs. Staff shortages, continuing cost inflation and service demand have intensified the call more effective and efficient use of scarce resources through integrated service models.
Benefits of integrated care
BENEFITS OF INTEGRATED CARE
POORLY INTEGRATED CARE
Better patient experience
Duplication and gaps in service and infrastructure
Improved outcomes
Under- and over-use of resources
Improved adherence to treatment
Medical errors and adverse events
Improved quality of life
Accessibility problems and discontinuity in care
Improved efficiency
Unmet healthcare needs
Delivering integrated care is essential to improving outcomes for people who use services in low threshold settings. Treatment services are most effective and attractive to PWID patients when they are: easily available; voluntary; unconditional; free of any legal consequences; address individual needs; and different harm reduction and treatment services are available in one place (syringe/needle exchange, OST, ARV, HCV treatment etc). The most successful linkage-to-care rates were seen in settings where testing, care, and treatment are provided in one place.
This test-and-treat model eliminates the need to refer patients to an outside care provider, except in extenuating circumstances. In collaboration with public health agencies and other service providers, community health centers are optimally positioned to play a pivotal role in expanding access to recommended testing, care, and treatment for people who use drugs.
KEY MESSAGE
TESTING + DIAGNOSIS + TREATMENT + CARE + REHABILITATION + HEALTH PROMOTION = BETTER ACCESS, QUALITY, USER SATISFACTION AND EFFICIENCY.
INTEGRATION MEANS TO IMPROVE SERVICES INNCLUDING ACCESS TO THEM, QUALITY, USER SATISFACTION AND EFFICIENCY.
„ONE SIZE DOES NOT FIT ALL“ – INTEGRATED HEALTHCARE BRINGS TOGETHER DIFFERENT TREATMENT APPROACHES FOR MORE DIVERSITY AND EFFECTIVE OUTCOMES FOR INDIVIDUALS AND SOCIETY AS A WHOLE.
People who use drugs (PWUD), including people who inject drugs (PWID), are marginalized and stigmatized in most societies and are often at increased risk of acquiring and transmitting HIV, hepatitis, and other blood-borne pathogens. These populations are hard to reach and often the least able to access and the least likely to utilize HIV prevention, care, and treatment services. Therefore, HIV prevention programs need to be developed or tailored to effectively target, reach, and address the particular needs of PWUD. Any patient whose socioeconomic conditions or lifestyle makes it difficult to access health services, self-administer treatment, and attend regular healthcare appointments.
In addition to the type of integration, strategies for improving the links between services may be linked-widely varying goals: some strategies are mainly implemented to reduce costs, while others additionally focus on quality, access, and user satisfaction. Integrated care may be deemed successful if it: contributes to better care experiences; improves care outcomes; or delivers services more cost-effectively. Without integration at various levels, all aspects of health care performance can suffer. Patients get lost, needed services fail to be delivered, or are delayed, quality and patient satisfaction decline, and the potential for cost-effectiveness diminishes.


